In the rapidly evolving landscape of healthcare, the need for well-prepared medical professionals has never been more critical. As patient needs become increasingly complex and diverse, medical education must adapt to ensure that future healthcare leaders are equipped with the necessary skills and knowledge. This article explores the evolving trends in medical education and highlights key reforms in the medical curriculum that are shaping the next generation of healthcare providers.
Evolving Trends in Medical Education: A Comprehensive Overview
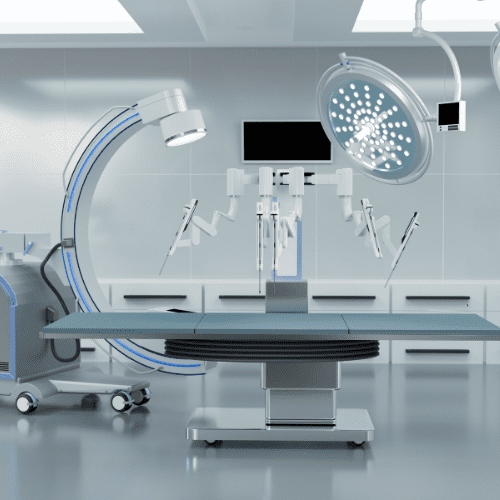
The world of medical education is undergoing significant transformation driven by advancements in technology, pedagogical strategies, and a deeper understanding of the healthcare landscape. One of the most notable trends is the integration of technology into the curriculum, encompassing simulations, telemedicine, and online learning platforms. Virtual reality (VR) and augmented reality (AR) are being utilized to create immersive learning environments that allow students to practice procedures in a safe, controlled setting. This not only enhances clinical skills but also fosters critical thinking and decision-making.
Another key trend is the emphasis on interprofessional education (IPE), where medical students collaborate with peers from various healthcare disciplines. This approach emphasizes teamwork, communication, and mutual respect, preparing future healthcare leaders to work effectively within multidisciplinary teams. As healthcare becomes increasingly collaborative, understanding the roles and responsibilities of different professionals is vital to delivering comprehensive patient care. IPE also cultivates a sense of shared responsibility for patient outcomes, reinforcing the importance of holistic care.
Additionally, there is a renewed focus on social determinants of health and health equity in medical curricula. Recognizing that patient care extends beyond clinical settings, educators are incorporating topics such as cultural competence, community health, and public health policy into the curriculum. By understanding the broader context of health, medical students can better address the unique needs of diverse populations and contribute to reducing health disparities. This shift not only enriches the educational experience but also aligns with the evolving role of physicians as advocates for health equity.
Key Reforms in Medical Curriculum for Future Healthcare Leaders
One of the most critical reforms in medical education is the shift from a traditional lecture-based approach to a more active, learner-centered pedagogy. This includes problem-based learning (PBL) and case-based learning (CBL), which encourage students to engage with real-world scenarios and develop problem-solving skills. Such methods promote deeper understanding and retention of knowledge, equipping students to tackle complex clinical challenges. Furthermore, these active learning strategies foster collaboration and communication skills that are essential in the healthcare environment.
Another significant reform is the integration of a competency-based education (CBE) framework. CBE focuses on ensuring that medical students acquire specific competencies necessary for successful practice, rather than solely relying on time-based training. This reform allows for personalized learning paths, enabling students to progress at their own pace and ensuring that they achieve mastery in essential areas. By clearly delineating competencies related to clinical skills, professionalism, and communication, medical educators can better prepare students for the realities of patient care.
Lastly, the incorporation of well-being and resilience training into the curriculum is gaining traction. Recognizing the high levels of burnout and mental health challenges faced by healthcare professionals, medical schools are now prioritizing the well-being of their students. Programs that focus on mindfulness, stress management, and self-care are being integrated into the curriculum to equip future leaders with the tools they need to maintain their own mental health while providing high-quality care to others. This holistic approach acknowledges that the well-being of healthcare providers is intrinsically linked to patient outcomes and health system efficiency.
In conclusion, the reforms in medical curriculum reflect a commitment to evolving educational practices that meet the demands of a changing healthcare landscape. By embracing technology, fostering interprofessional collaboration, and emphasizing health equity, medical education prepares students not only to excel as clinicians but also to be compassionate and socially responsible leaders. As we continue to adapt to the challenges of modern healthcare, these reforms will play a pivotal role in shaping the future of medicine, ensuring that healthcare leaders are well-equipped to face the complexities of patient care.